Victoria Samaila lost two daughters to cholera
Nothing at the camp makes the existence of the IDPs enjoyable. The shattered roofs above their heads and the naked rooms expose them to deadly infections. The Kuta IDP camp looks unfit for humans to dwell in.

Having received no medical intervention from the government in the past two years, the IDPs are now left to cater to themselves, leaving them with the option of using self-discovered leaves and tree bark for medication.
At Kuta IDP camp, a small building which served as a medical facility has now become empty with nothing medical in sight. TheCable understands most of the IDPs nurture preventable diseases which could be easily treated with proper medication.

DISTANCE OF ACCESSING HEALTHCARE
Advertisement
From 2021 till date, about 14 IDPs, which includes more women and children, have died of various avoidable diseases at the Gwada camp, according to camp officials.
Habibu Kurebe, the desk officer, said they rely mostly on private hospitals but often receive incomplete treatment owing to lack of money.
Kurebe said the women’s hospital where they, sometimes, visit doesn’t always have medical experts to attend to them.
Advertisement
“It is not every time you go there you will meet the nurses or doctors. They usually leave the facility very early,” he said.
Kurebe said the only government hospital is at Kuta, which is about 40 minutes drive away from Gwada town.
“They don’t have money; getting money for transportation to the general hospital is a big problem,” he added.
“About 1,500 IDPs are currently living in Gwada camp and the government only brought some relief items during a cholera outbreak in 2021.”
Advertisement
CAUSES OF DISEASES AT IDP CAMPS

Godwin Ntadom, the chief epidemiologist of Nigeria, said the poor environmental condition IDPs dwell in contributes to the disease prevalent among them.
Commenting on the persistent coughing discovered among the children in the camp, Ntadom said it could be tuberculosis, adding that it is a communicable disease.
“From what you have described, probably we will be thinking of tuberculosis since the cough has been there for a long time. It is also very dangerous to do diagnosis like that without going to the laboratory. Get a sample to the lab but there are so many other things that can cause coughing,” he said.
Advertisement
“The IDP camp is already a compromised setting, overcrowding, pests, and mosquitoes are not controlled. Some bigger IDP camps, I don’t know the one you went to but they usually have a medical facility, a clinic.
“It is not unusual to see tuberculosis, cholera, malaria and etc., at the IDP camp and all these are a result of the compromised environment, no adequate facilities, overcrowding.
Advertisement
“They live in an enclosed environment. So, if one of them has a cough, almost all of them can develop a cough. If one of them has measles, those who are not vaccinated, develop measles.
“To curb diseases, good water needs to be provided. Construct boreholes because most of the diseases are water-related, provide insecticide nets, and children should be properly immunised. After living in the IDP camp for long, they suddenly become a baby factory. So, they need a lot of education on family planning.”
Advertisement
ABANDONED MEDICAL FACILITY
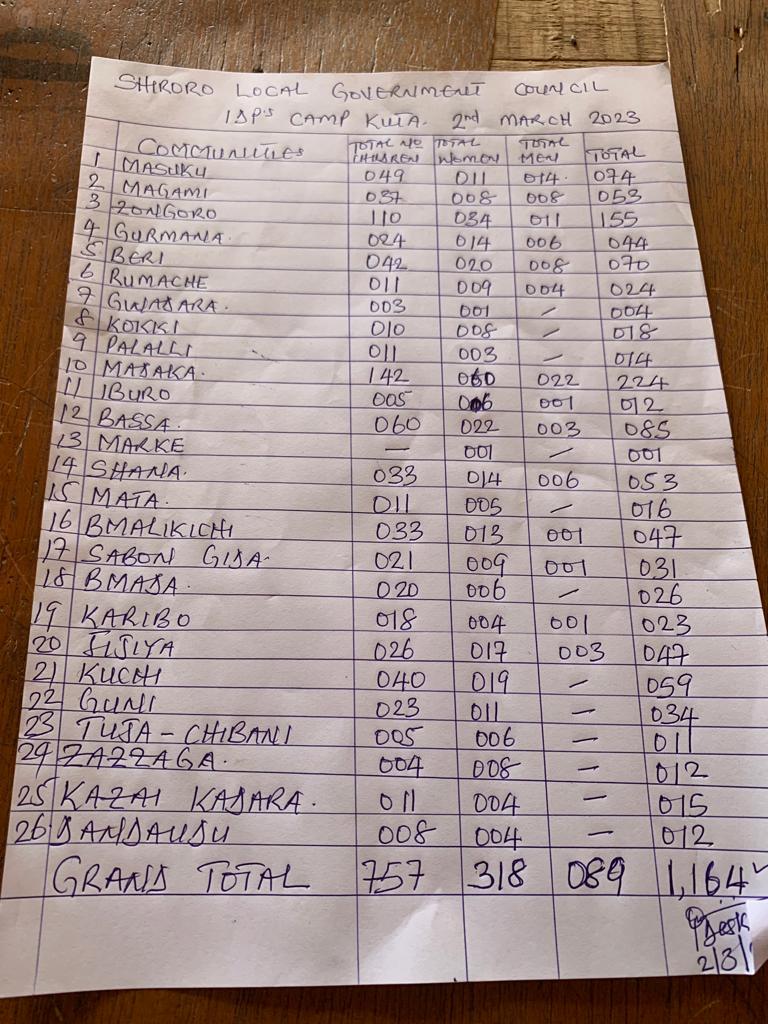
As of March, over 1,000 people from 26 communities were living in the IDP camp in Kuta. In the camp, a small clinical space was created to attend to sick IDPs, but it is currently scanty — no drugs or medical kits to help the sick inhabitants. According to Idris Wakili, the assistant desk officer, the space has been abandoned for more than two years now.
Advertisement
“Some of them, when they exhibit chronic symptoms, we refer them to the General Hospital here. To be sincere, accessing healthcare is very difficult for the IDPs because most times, we pay for their treatments. We used to have a doctor called, Hamza Idris, who usually come to check on them but we have been managing to help them individually.” Wakili said.
“Since the camp was set up in 2018, the camp has lost a lot of people, and even the camp environment and structure was not conducive for them. We have recorded deaths of infants due to malnutrition and women dying or losing their babies during childbirth.”
He said eight children have died of sicknesses such as typhoid, stomach pain and malaria in the IDP camp, while three other kids died of malnutrition in the past two years.
LOCAL AUTHORITIES NOT HELPING
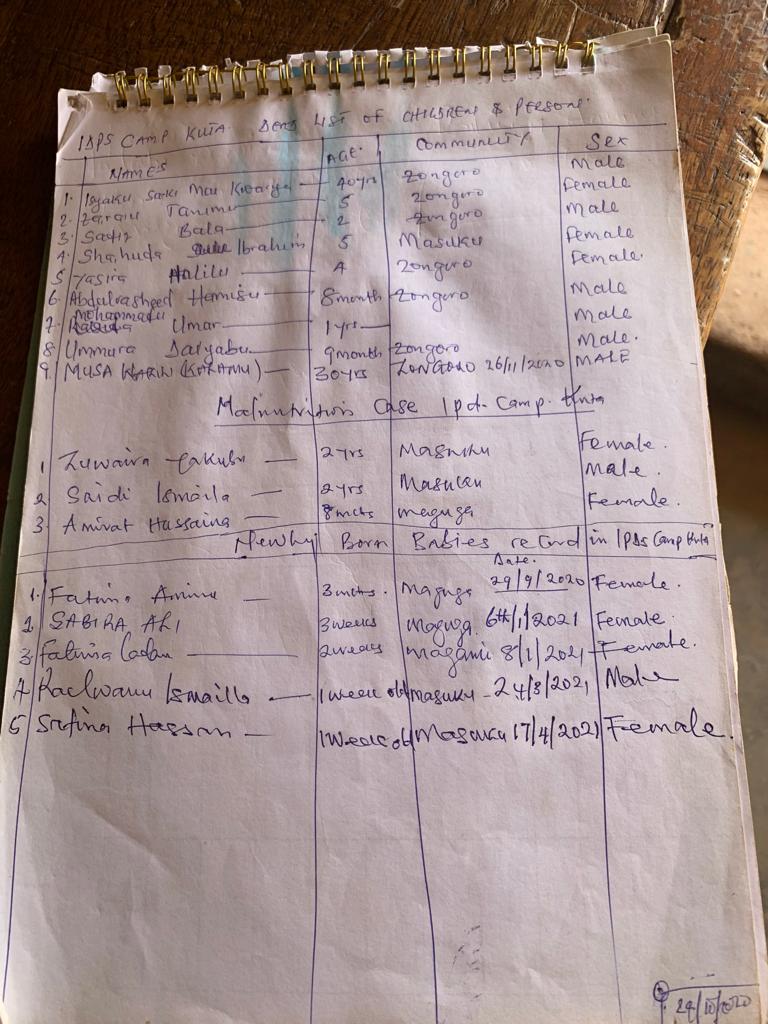
For about two years now, Wakili said seven children including infants died of unknown illnesses in Kuta camp. He said some of the children exhibited symptoms of stomach pain and fever, adding that three more female children died of malnutrition.
“The previous government at the LGA was not helping. When the new local council chairman assumed office recently, we reached out to him about water and two weeks ago, he fixed the borehole,” he added.
“The last time we had drugs in this facility was two years ago when an organisation made donations. The Development Initiative of West Africa (DIWA) was the last organisation that distributed drugs to the camp. It is a pathetic situation here.”
‘IDPs NOT OFFICIALLY REFERRED TO GENERAL HOSPITAL’

Abdulsalam Abdulsalam was recently transferred to the General Hospital in Kuta as the general doctor. Since he assumed the position three months ago, he has only encountered a single severe case of an IDP rushed into the emergency unit.
The patient had prolonged labour and was brought into the facility exhausted as she had lost a lot of blood.
“There was a case of an IDP brought in here two weeks ago. She was bleeding severely and the baby died in the process. So, we just do what we can. If you are talking about a proper referral from the IDP camp, we have not seen it. But we have seen some IDPs. We were able to save the mother, at least,” he said.

Speaking on the cough situation at the Kuta camp, he said: “Being in an IDP camp, the most common illness is malnutrition. The same child might be having tuberculosis, whooping cough and so on.”
“It will be better that when you have such symptoms, you come to the hospital so we can prevent transmission to others. The majority of things that causes cough are communicable but we don’t receive official referrals from camp officials. Even when they come here, we don’t usually know they are IDPs.”
SHOULD AN IDP CAMP HAVE A MEDICAL FACILITY?
For more than five years, IDPs in Niger have lived in temporary camps provided by the government. These camps have now become home to thousands of IDPs as the security challenges in their various communities continue.
The African Union Convention for the protection and assistance of IDPs in Africa (Kampala Convention) under article 5 on the obligation of state parties said: “State parties shall provide sufficient protection and assistance to the IDPs and where available resources are inadequate to enable them to do so, they shall cooperate in seeking the assistance of international organisation and humanitarian agencies, civil society organisation and other relevant actors. Such organisations shall offer their services to all those in need.”
Since 2014, IDPs in Kalar and Arbat (Syria and Iraq) have enjoyed free access to healthcare facilities built in their temporary camps. For about ten years now, over three million Syrian refugees and Iraqi IDPs have been living in Iraqi Kurdistan as a result of the conflict in their countries.
Emergency Belgium, a Belgian affiliate of Emergency – a non-governmental organisation with the United Nation Department of Public Information as its official partner — have constructed seven medical facilities for the IDPs and refugees in Arbat camp. The clinics were built to separately attend to Syrian refugees and Iraqi IDPs while another was opened for adults and pediatric patients. The clinics offer essential services such as obstetrics and gynaecology as well as vaccination programmes.
The organisation had, through the initiative, created job opportunities for local people with trained health promoters while 72 local members of staff both medical and non-medical were employed to work in the clinics. In 2017, the organisation transferred its operational responsibilities of the facilities to local healthcare authorities as part of the government’s plan to support refugees and IDPs to return to their countries and original communities.
WHAT IS SEMA DOING?
Ibrahim Hussaini, spokesperson of the Niger State Emergency Management Agency (SEMA) said providing medical services and facilities is the responsibility of the agency but the IDPs’ stay at the camps is not static.
According to him, the IDPs come and go when they hear of relative peace in their communities, adding that some of them leave with the relief materials given by SEMA who may now have to distribute more items for a new batch coming to resettle in the camps.
But most of the IDPs who spoke with TheCable said they have been living in the camps for the past five years.
Speaking on funding for the health of the IDPs, the SEMA official said: “What we do is that anytime we are writing a memo for review participants, we include money for drugs and other treatment aids and as soon as the money is given to us, we remove it completely and give it to the ministry of health to take charge but the money is taken from SEMA.”
“We cannot quantify that amount because of the fact that we have been writing so many memos and if we want to do that, we have to go back to all the memos and begin to extract all the money. What we do is we come around, go to the camp, check their needs, and include it in our memo.
”Yes, it is the responsibility of SEMA to coordinate the ministry of health for medical services and facilities to the IDP camp. We have departments in ministries (MDAs) responsible for providing all this assistance. Our own is to coordinate the human resources and also material resources.
“We go on intervention on a regular basis but the problem we are having with the IDPs is that their situation is not static.”
But the camp official told TheCable that only the Development Initiative of West Africa (DIWA) had visited the camp with medical items for the IDPs.
‘OUR JOB IS TO ATTEND TO DISEASE OUTBREAKS’
Ibrahim Idris, director of public health, Niger state ministry of health, said that all funding for the IDPs healthcare is done by SEMA.
“IDP camps are the responsibility of SEMA. We only come in when there are health issues. Sometimes, there will be an IDP camp somewhere and there are no health issues, they may not even inform us there is a camp somewhere. When any of our principals are coming because, at that point in time, they want to show they are working with everybody. They are supposed to be working with us. We have an emergency operation centre. We try as much as possible to do our emergency responses,” Ibrahim said.
Though Ibrahim said SEMA is responsible for funding health-related interventions to the IDP camp, SEMA officials had told TheCable that the fund for healthcare for IDPs after allotted is removed and given to the ministry of health.
The public health director said the camp is supposed to be a temporary site but has now been turned into a permanent home by the IDPs.
“How often we visit the camp is how often SEMA tells us. They are no longer in camps, they have indirectly turned that place into a home,” he said.
“There is an outbreak of diarrhoea. What causes diarrhoea and vomiting is not under our control. If the water board did not make a supply and people take contaminated water and there is a cholera outbreak, who do they call? They will say ministry of health should come and take care of it.”
Though he said the health ministry goes to the camps when there is a disease outbreak, many IDPs including children have reportedly died due to the cholera outbreak in the camp since 2021. but nothing has been done to stop the spread.
“Issue of having a medical facility for IDPs, we can’t allow our staff to remain there when the IDPs don’t stay there. If they need medical services, the camp manager can inform the local government as they are closer to them.”
NGO WORKING FOR IDPs
Daoud Kenneh, chief executive officer of DIWA, told TheCable that the organisation usually takes medical packs and other hygiene necessities to IDPs in Gwada and Kuta towns.
Kenneh said the organisation also constructed toilets for IDPs in Kuta camp, adding that most of its projects are usually funded solely, but NEMA is informed of their activities in the state.
“On two or three occasions, we have done medical outreach. We mobilised medical professionals to the camp. We also involve SEMA; of course, they are not part of it. We recently provided solar boreholes for hygiene and we also constructed latrines to prevent health hazards like cholera,” he said
“We try to do these things with the consent of SEMA but of course, they don’t contribute to it but we feel they are the host so we take one of them with us. We have done a number of medical outreach, we take it to them.”
TheCable understands that the IDPs have not received intervention from the government for about two years, while many camps have been left in poor condition. The IDPs have also been left at risk of many deadly diseases.
As of November 2021, there are over 50,000 displaced persons living across LGAs in Niger state. In many other camps across Nigeria, children have reportedly died of measles, typhoid, malnutrition, and cholera among other preventable diseases over lack of accessible medical services.
Like in the case of Syrian and Iraqi refugees and IDPs and as stated in the African Convention for IDPs protection laws, collaboration with civil society organisations (CSO) will help in providing better health services to IDPs through working arrangements and intervention to curb the spread of diseases causing death in the camps.
NIGER HEALTH BUDGET 2020 – 2023
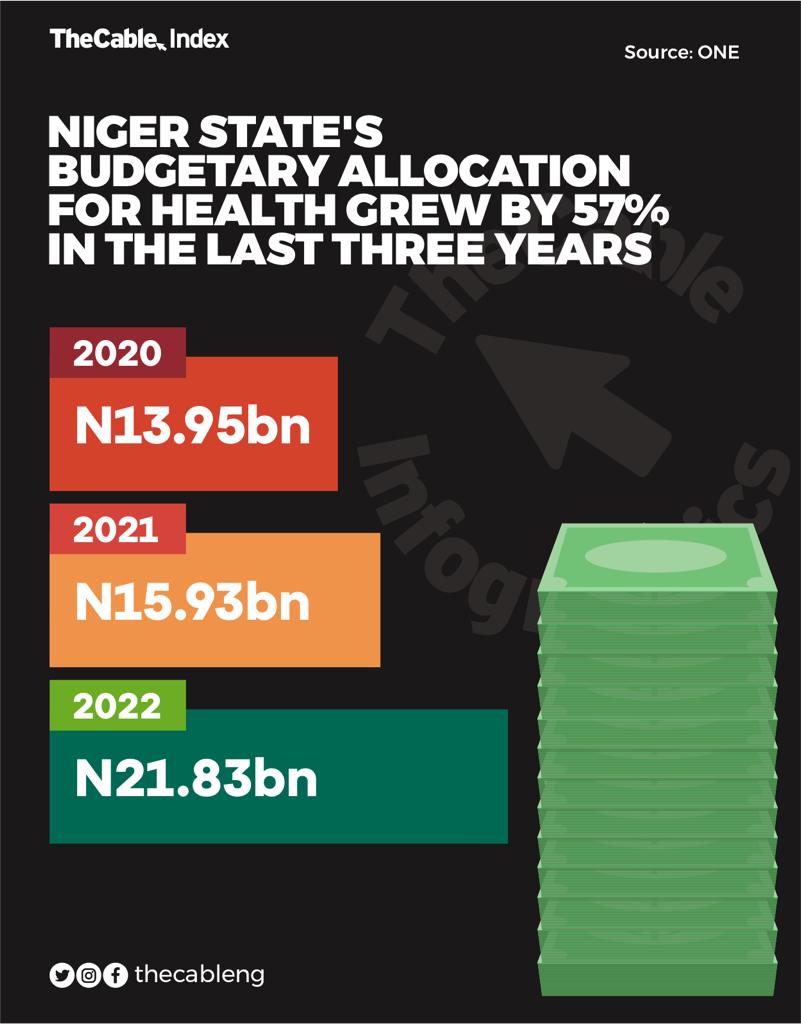
According to the data and analysis by ONE, a global movement campaign focused on ending extreme poverty and preventable disease by 2030, Niger state has consistently increased budgetary allocation to the health sector from 2020 to 2023 like 13 other states.
In 2020, the state allocated N13.95 billion, 15.93 in 2021. The budgets growth stands at 14.2 percent,
In 2022, the health budget rose to N22.83 billion, while the growth between 2021 to 2022 increased to 37.0 percent. However, from 2020 to 2022, the health allocation increased by 56.5 percent.
Despite this increase, many citizens still find it difficult to access quality healthcare services in the state.
This report was supported by the Wole Soyinka Center for Investigative Journalism (WSCIJ) under its Report Women! Female Reporters Leadership Programme (FRLP), champion building edition.
Add a comment






