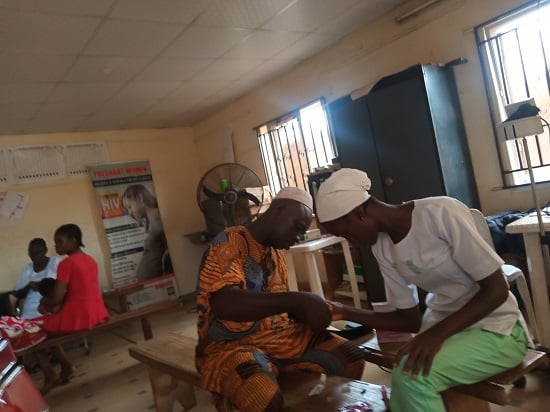
Without PPE, a health worker collects blood sample of an elderly man at Ajaka PHC, Sagamu LGA
Across several communities in Ogun state, the federal government’s Basic Health Care Provision Fund (BHCPF) is improving access to healthcare, but its success is threatened by insecurity, shortage of personnel and low awareness.
On a drab Tuesday morning in July, Ibidun Ajibade, a staff at Igan health centre in Ijebu-East LGA, Ogun state, wore a smiling face as she turned on the newly-acquired solar light in the facility.
Her excitement did not immediately ring a bell. But as the reporter would later find out, it tells a story of hope.
For six years, the facility grappled with darkness owing to a lack of electricity, among other challenges, which, according to her, affected its effectiveness.
Advertisement
Since October 2021, however, the facility has witnessed a significant facelift, with the support of the BHCPF — a multi-million naira intervention from the federal government.
“For about six years now, we’ve not had a public supply of electricity, but through the BHCPF, we have that. We also have solar lights provided to support our operations. The scheme also got us other items such as mopping sticks, chairs, fans, and drugs,” she said.
At Ajaka primary health centre (PHC) in Sagamu LGA — about 96.5 km away — Blessing Oluwole, an expectant mother, exudes an unusual calmness while waiting to be called upon by Onihale Comfort, one of the only two midwives at the facility.
Advertisement
Blessing’s first visit to the PHC was in April when she took ill. Her experience at the facility was enough to convince her that it was the right place for antenatal care.

“The first time I visited here, I was sick. I got good treatment without paying much. So, when I became pregnant, I decided to come here again. Since I have been coming for pregnancy treatment, it’s been a nice experience,” Blessing said.
Like Blessing and Ibidun, health workers and residents in the state say the BHCPF scheme has raised optimism among the people since its implementation.
THE GAME CHANGER
Advertisement
The BHCPF was established under section 11 of the National Health Act (NH Act), 2014, as a key principal funding mechanism for achieving universal health coverage (UHC) in Nigeria.
The scheme seeks to achieve at least one fully functional public or private primary health care (PHC) facility in each political ward, at least 30 per cent of all wards over the next three years, 70 per cent within five years, and 100 per cent within seven years.
It also aims to reduce out-of-pocket expenditure by 30 per cent in five years, increase financial risk protection through health insurance, and raise the country’s life expectancy to at least 60 years over the next 10 years.
The initiative is derived from about one per cent of the consolidated revenue fund (CRF) and contributions from donor agencies.
Advertisement
The fund is implemented through three gateways namely: the National Health Insurance Scheme (NHIS), the National Primary Health Care Development Agency (NPHCDA) and the National Emergency Medical Treatment (NEMT).
According to the act establishing the scheme, the NHIS is to get 50 per cent while the NPHCDA gets 45 per cent. The remaining five per cent goes to NEMT, which caters for outbreaks and emergency responses.
Advertisement
The NHIS, for instance, contains the Basic Minimum Package of Health Services (BMPHS), which, according to Enahire Osagie, the minister of health, currently provides free healthcare for about 753,999 “poor Nigerians”. That of the NPHCDA gateway consists of funding for essential drugs, vaccines, and consumables, maintenance of primary healthcare facilities, equipment, transport and personnel.
Under the scheme, officially launched by President Muhammadu Buhari in January 2019, one PHC is selected from each ward and gets N300,000 per quarter. To assess the fund, each state is expected to pay a required counterpart fund and meet other criteria which include the establishment of a state primary health care development board.
Advertisement
In 2019, the federal government disbursed a total sum of N13.8 billion for the BHCPF, with the NPHCDA accounting for N5.5 billion of the fund.

Advertisement
Ogun became a part of the initiative in October 2021. Data from the NPHCDA showed that out of the 237 wards in the state, 169 (representing 71 per cent) health facilities have been verified to receive the funds.
In 2022, the federal government released N28.59 billion across the 36 states in Nigeria and the federal capital territory (FCT). Osagie had, in August, said since the initiative was launched in 2019, N56 billion out of the N89 billion released for the project has been disbursed.
Visits to several of the facilities at Sagamu, Abeokuta North, Ifo, and Ijebu-East LGAs revealed that the initiative is bringing succour to residents, particularly the aged, children and pregnant women.
“I am happy that my child has access to good and free healthcare whenever she’s sick,” Deji, a mechanic in Ogbere, Ijebu-East LGA, said while lauding the initiative.
Across the LGAs, officials said the intervention has increased the enrolment of patients as well as the number of health personnel at the PHCs.

The scheme has also provided a source of livelihood to ad-hoc health workers engaged by the facilities. One of the ad-hoc workers is Olorunda Eunice, who graduated from the Rufus Giwa Polytechnic in Owo, Ondo state. Eunice was recruited as an ad-hoc desk officer at Ajaka PHC under the BHCPF.
Her monthly stipend of N15,000 may be far lesser than the approved national minimum wage of N30,000, but it is giving Eunice and her little daughter a lifeline after hunting for a job for months without any success.
Moreso, the intervention has improved infrastructure in the PHCs. Before now, the sight of a gathering cloud signals a nightmare for health workers and patients at Elega PHC in Abeokuta North LGA; Ojodu Abiodun PHC in Ifo LGA; as well as Latawa PHC in Sagamu LGA.
From a bushy environment, and defaced walls to sagging and leaking roofs, the facilities, like several others in the state, have seen better days. But the narrative is changing with a series of renovations facilitated by the BHCPF. Under the scheme, PHCs also engaged cleaners to maintain hygiene around the facilities.

“Our roofs are leaking seriously. We are embarking on a series of innovations with money gotten through the fund,” Lemoha, the officer-in-charge of Elega PHC, said.
Olaitan Olumide, an official with Justice Development And Peace Commission (JDPC), a non-governmental organisation, said the BHCPF will help tackle the country’s high maternal mortality rate.
“The BHCPF is a welcome intervention by the federal government and it is coming at the right time, knowing fully well that maternal mortality rate in Ogun State and in Nigeria generally is increasing,” he said.
INSECURITY, LOW AWARENESS… FACTORS THREATENING SUCCESS OF BHCPF IN OGUN
While the BHCPF is improving the infrastructure and access to healthcare, there is a major challenge in the PHCs visited: the shortage of personnel to complement the progress made by the intervention.
In 2009, the federal government introduced the Midwives Service Scheme (MSS) to address the shortage of skilled health workers in rural communities by temporarily redistributing midwives from urban to rural communities. The scheme also recruits new graduates from schools of midwifery, unemployed midwives and retired but able midwives for community service.
But the programme stopped in 2013 in Ogun and several other states. The development has dealt a major blow to access to healthcare in the state.
Lawal Ayomide, a motorcyclist in Ogbere, Ijebu-East LGA, almost lost his life when he had an accident on January 11, 2022, and was rushed to Ogbere PHC, but nobody was on the ground to attend to him.

“When I was rushed there, it took about 30 minutes before I was attended to. The accident was serious and I felt I was going to die,” he said while showing the reporter scars of the incident.
“The issue with the centre is the availability of the health workers. Sometimes, when we go there, it’s the security that would call the nurse,” he said.
In Atoyo, another community in the same LGA, the story is not different. Odelana Titilayo, secretary of Atoyo community, and his family are enrolled in the BHCPF and usually get free drugs — courtesy of the state health insurance scheme — whenever they visit the PHC.
But the unavailability of health officials is a major problem for him and several others in the community. “They (the officials) don’t collect money from us. The drugs are free. However, there are several challenges. In the first place, there’s a shortage of staff. As a result, we usually call the health workers on the phone before they will come around,” Odelana said.

Residents of the community said in the case of a health emergency at night or when a pregnant woman is about to put to bed, they usually rush them to Itele, a neighbouring community, which is about 4 kilometres away.
When this reporter visited the facility, it was under lock, while a woman who said she came for malaria treatment was seen leaving the vicinity in annoyance.
Baale Adekomaya, a traditional ruler in the community, said due to the non-availability of health workers, a lot of people in the area don’t visit the facility anymore.

Residents are not the only ones bearing the brunt of the shortage of personnel. “I am the only midwife here. The work is too much. I always try to delegate responsibilities as much I can,” Odunayo, the officer-in-charge of Enugada PHC in Abeokuta North LGA, lamented.
From Latawa and other PHCs in Sagamu LGA to Ajuwon PHC in Ifo LGA, health workers complain of being exhausted daily due to excess workload — a challenge which would have been addressed by the MSS initiative.
Beyond the shortage of health personnel, the BHCPF is also threatened by inconsistencies in the disbursement of funds. While some of the eligible PHCs in the state have received the first and second tranches of N301,000 each, others complained they have not gotten any funds since the programme commenced.
“We haven’t received any funds since October last year. I have made several complaints without any tangible result,” the officer-in-charge of Odoladalepo PHC in Ijebu-East LGA said.
PHCs that got the first and second tranches also lamented that since March, they are yet to receive additional funding.
V.O Adeuja, the officer-in-charge of Ajaka PHC, said the development has made it difficult for the facility to pay its ad-hoc staff the N15,000 monthly stipend and sustain other operations.
“We got the fund in October last year till March, which was N601,000 in total. The fund finished in April. We have not received anything for May and June. The only staff that we employed via the fund, it’s been difficult to pay her,” she said.
“Then, we need some things that we ought to continue, such as electricity bills — which we have been paying ourselves, that one is lacking now. The drugs we usually get with the fund are also no longer available.
“With the fund in place, things were easy for our patients but since it stopped, we don’t know what to do anymore. It’s like we have to go back to how we were managing before until they answer us.”
Several of the ad-hoc staff like Eunice also decried the non-payment of their monthly stipends.

In addition to the delay in disbursement, the fund is also docked by issues of non-flexibility. Several PHCs complained of not getting the support of the ward development committee (WDC) to use the fund to address urgent needs not originally captured in the budget plan.
At Ajuwon PHC, Omojola Adebimpe, the officer-in-charge, said the facility’s urgent needs are not being addressed due to the non-flexibility of the programme.
“The issue here is the signatory…the person in charge of the money is different from me who is in charge of the facility. So, she would not be able to feel my pain. We’re not the only one experiencing it; so if the issue of the signatory is dealt with, the programme would be more effective,” she said.
“We have issues with releasing the money and changing signatories. But our ward focal person is afraid of issuing the cheque. The money is just there. In fact, there’s a fence project we’re meant to execute for security and other needs which are not captured in the business plan. I complained, but nothing was done. We’re just seeing that we are getting the money, but it’s not being maximised.”
At Ibido PHC in Sagamu LGA, a similar issue exists. An official at the facility said although the centre lacks water, the WDC said it cannot fix the damaged borehole from the fund given to them.
“The major issue we have here is water. The only borehole here isn’t functional. But they said we can’t do it from the fund that was given to us,” the female official said.
There is also low awareness of the BHCPF in some of the communities visited.
At Ajuwon PHC, Adebimpe lamented the low turnout for the programme, particularly among pregnant women.
“We’re getting enough people for the programme as we expected. It also appears that pregnant women weren’t captured during the enrolment process because since the programme started, we’re yet to record a birth under BHCPF and I usually get worried about that. So, we’re not seeing them,” she said.
“WE ARE AFRAID OF SNAKES, MOSQUITOES, INSECURITY”
In several of the PHCs visited, health workers also complained of insecurity and poor amenities which makes it difficult for them to carry out efficient service delivery.
At Elega PHC in Abeokuta North LGA, health officials said pregnant mothers and other patients do not stay long at the facility due to a lack of security, mosquitoes and snakes.
“Most of our patients don’t stay because of insecurity. We are always in darkness at night. Mosquitoes and other reptiles including snakes usually enter the facility,” Lemoha, head of the PHC, said.

“When we resume work in the morning, we’re always battling mosquitoes. If a patient comes here without malaria, such a person is likely to have it when leaving just because of the mosquitoes. This is far from an ideal laboratory,” a lab scientist at Enugada PHC, also within the same LGA, said.
In Atoyo and Igbaga PHCs in Ijebu-East LGA, the situation is the same. “How do you expect me to sleep in this condition at night? The louvres are broken, no mosquito nets and no security. With the situation of things in the country, no one can sleep here. If these can be fixed, I can manage it,” an official at the facility said.
COMMISSIONER: WE’RE DOING OUR BEST TO IMPROVE THE SYSTEM
Reacting to findings by the reporter, Tomi Coker, the state commissioner for health, said efforts are in place to address the challenges facing the implementation of the BHCPF in the state.
Coker said the state has a total of 521 PHCs, and out of this, 196 facilities are enlisted for the BHCPF. The commissioner said the number of PHCs benefitting from the initiative will soon be increased to 236 when the facilities meet the necessary requirements.
“We intend to increase the PHCs getting the BHCPF to 236. The issue is that you have some of them that have not met the criteria. They are meant to register patients for insurance and when we went around registering patients; they didn’t,” the commissioner said.
Coker said the state has an insurance scheme in place to ensure free drugs are given to patients and make the BHCPF initiative more effective.
“The PHCs operating BHCPF are available to the general public. People who are not registered for the insurance scheme are to pay for the drugs. However, those drugs must be cheaper than the ones they get outside because we provided them at a very reduced rate,” she added.
“But those that are part of the state’s insurance scheme get free drugs. They should not pay a dime, and if you have PHCs where people on insurance are paying for drugs, please let me know.”
The commissioner added that the state has embedded the MSS template into the BHCPF to address the shortage of personnel and improve access to primary healthcare across the PHCs, since the intervention from the federal government failed.
“So far, we have employed 67 midwives. We want to ensure we have midwives in every single PHC, but will that be possible? Perhaps not, because the midwives are not out there to be employed.” the health commissioner stated.
Also speaking, Elijah Ogunsola, the executive secretary of the state primary health care development board, said there are several measures to increase awareness about the BHCPF and the state insurance scheme.
On the non-flexibility of the fund to meet emergency needs, Ogunsola said cheques can only be issued for projects captured in the plan submitted by the PHCs and approved by the health commissioner.
“We know with time, our people will improve. For them to procure, there should be a business plan approved by the honourable commissioner before they move ahead. So, they would have stated what they want to do and that is what the audit would do,” Ogunsola said.
“We have auditors at three different levels. We have auditors from the office of the account-general of the federation (AGF), the NPHCDA, while our own auditors also visit the PHCs to ensure that what they put in their business plan is in line with cheques that they have raised.”
Ogunsola said the board also has a monitoring team in place to ensure accountability and transparency in the utilisation of the funds given to the PHCs.
This report was published with support from the International Budget Partnership (IBP) and the International Centre for Investigative Reporting (ICIR).
Add a comment





