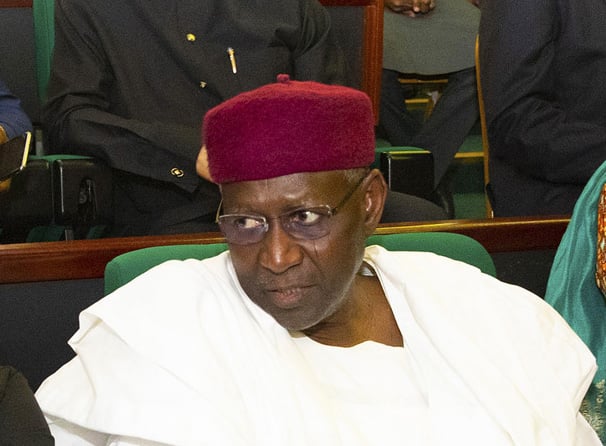
PRESIDENT BUHARI METS CORONAVIRUS COMMITTEE ON THE ECONOMY B. President Muhammadu Buhari receives briefing from the Minister of Finance, Hajiya Zainab Ahmed during a meeting with the Presidential Committee to Review the Impact of Coronavirus on the Economy held at the State House Abuja. PHOTO; SUNDAY AGHAEZE. APRIL 2 2020
BY ADIE VANESSA OFFIONG
Nigeria had been waiting for it, expecting it, anticipating it. But no one knew exactly as it came in. Only in hindsight would the country piece together the story of an Italian man who arrived by air in Lagos on March 24, infected with SARS-CoV-2.
By four weeks later, 1,337 people had been infected, among whom 40 people had died, and 255 people had been discharged from hospital. The number of people released from hospital is encouraging but questions swirling about the virus are prompting concerns among Nigerians as to how prepared the country was for COVID-19.
Nigeria has been here before. In 2014, Patrick Sawyer, a Liberian-American man, flew in with our first case of Ebola. Then, as now, it took the alertness of Lagos to help combat the spread of a virus. However, Nigeria’s preparedness to prevent, detect and rapidly respond to public health risks has changed over the last three years.
In 2017, a Joint External Evaluation (JEE) of the country’s preparedness rated the country 39%. It meant Nigeria was “not ready for the next epidemic”. The JEE comes under review every five years, but two years after the first report, Nigeria has a mid-term evaluation. By then, the score was 46%, which meant that while Nigeria continues to show commitment to epidemic preparedness, the country had “work to do to prepare for the next epidemic”. The next, unfortunately, arrived in the form of COVID-19.
Advertisement
According to the mid-term report, currently, immunization is Nigeria’s area of strength – in part because of Nigeria’s emergency operations center and robust laboratory systems that can quickly diagnose infectious diseases. But Nigeria’s areas of gap include monitoring systems that can spot unusual health reports from local clinics, and trained disease detectives who are ready to be rapidly deployed when a new health threat is reported. Other gaps reflect the need to strengthen Biosafety and Biosecurity, National Legislation, Policy and Financing, Preparedness, Linking Public Health and Security Authorities, National Laboratory System, Emergency Response Operations, and Real-Time Surveillance.
Perhaps more indicative of Nigeria’s preparedness to deal with outbreaks is Lassa fever. From week 1 – 5 of 2019, there were a total of 794 suspected cases, and 294 confirmed cases, with 52 confirmed deaths. In the same period in 2020, there were 1,226 suspected cases, of which 365 were confirmed. This reflects a 21.5% increase in number of confirmed cases; and with 47 confirmed deaths in the same period in 2020, an 11% reduction in number of deaths. This indicates improved case management. But the increasing number of cases is worrisome and speaks broadly of the country’s preparedness to handle outbreaks such as Covid-19.
Both Lassa fever and Covid-19 outbreaks are raging side by side, but each is getting varied attention. Lassa fever has fallen off the news; Covid-19 has taken over. Covid-19 is all everyone is talking about these days.
Advertisement
The government imposed a lockdown on Lagos, Abuja and Ogun for a first two weeks, then another two weeks, before extending for one more week before a gradual easing of restrictions. State governments and the federal government are rushing to establish site isolation and treatment centres as the numbers change rapidly. International donors, individuals and corporates have thrown billions of naira in cash and kind into the coronavirus disease response. With testing capacity increasing and more people being tested, the number of confirmed cases continues to rise—sometimes over 100 a day.
Initial models that the government was working with predicted that Nigeria would record an estimated 2,000 confirmed cases in the first month after the index case. But it turned out to be 1,337. “This means that… the measures we have put in place thus far have yielded positive outcomes against the projections,” said President Muhammadu Buhari, in his third broadcast since the outbreak. “The proportion of cases imported from other countries has reduced to only 19% of new cases, showing that our border closures yielded positive results,” he added.
The Nigeria Centre for Disease Control (NCDC) has accredited 15 laboratories across the country with an aggregate capacity to undertake 2,500 tests per day across the country. That is up from just five laboratories with capacity for real-time polymerase chain reaction test on the network of reference laboratories of the NCDC back in January.
With livelihoods on hold, work on pause, movement on restriction, clearly, the actual impact of Covid-19 is beyond mortalities. Nigeria cannot afford an outbreak. According to Wellcome, “Four years ago, when Ebola struck in West Africa, $2.2bn of economic growth was lost in Guinea, Liberia and Sierra Leone. When Zika hit the Americas in 2016, the short-term economic impact was $3.5bn. When SARS spread through Asia in 2003, it had a significant impact on the affected countries’ GDPs, with a loss of $40bn.”
Advertisement
Given Nigeria’s large population, and high biodiversity, zoonotic diseases which constitutes the majority of emerging diseases among humans, will continue to emerge. The diverse and complex ecosystems in Nigeria facilitate the human–animal interface and predispose humans and animals to the risk of zoonotic diseases. The next outbreak may be worse than Lassa fever and Covid-19. It is far cheaper to prepare. The time to act is now.
Offiong is a freelance journalist with experience in investigative, science and development journalism. She is member of Health Systems Global, African Investigative Publishing Collective and the Center for Collaborative Investigative Journalism.
Views expressed by contributors are strictly personal and not of TheCable.
Add a comment