For these women in Osun, pregnancy comes with a heavy burden of fear – whether or not they will live to carry their babies. The poorly equipped community health centres offer uncertain hopes. Enduring the pains and anguish, they travel distances to towns where they can get affordable healthcare. TAIWO ADEBULU, who visited rural communities in the state, reports.
Simbiat went into labour in the wee hours of a night in October 2015. The pains were unbearable. Her husband, Taofeek Adekunle, sprang up from bed and hurled her on his motorcycle to the traditional birth attendant’s house. The twin babies came out alive, though premature. It was their first offspring and they forced a smile at the sight of the little creatures; but they knew all wasn’t well.
The chilly night and shrilly cries made them fear the worst for the duo who had arrived before the expected day. By morning, when the inhabitants of Tedo village in Osun state woke up, the babies were dead. Simbiat was inconsolable. In his bereavement, Taofeek consoled his wife and took her home, while the remains of the babies were immediately interred.
“As soon as my wife got pregnant again, I took her to Ede town to stay. There, she got good healthcare from a hospital and delivered a baby girl. She returned to the village two months later,” Taofeek said.
Advertisement
Tedo village has no clinic or healthcare centre. The closest village, Ponpola-Ede, has a healthcare centre that has been under construction for the past 15 years. Through communal effort, residents strove to put up the structure to meet immediate medical needs but it has been stalled due to insufficient fund.
Aside Tedo and Ponpola villages, many rural communities in Osun state are battling with poor access to adequate health care. While it’s hard for most of these rural dwellers to get proper medical attention, the ones in major towns enjoy easy access to health services at any time of the day. Although the hospitals and health facilities at these major towns may not be fully equipped, they offer hope of getting immediate services without stress.
Advertisement
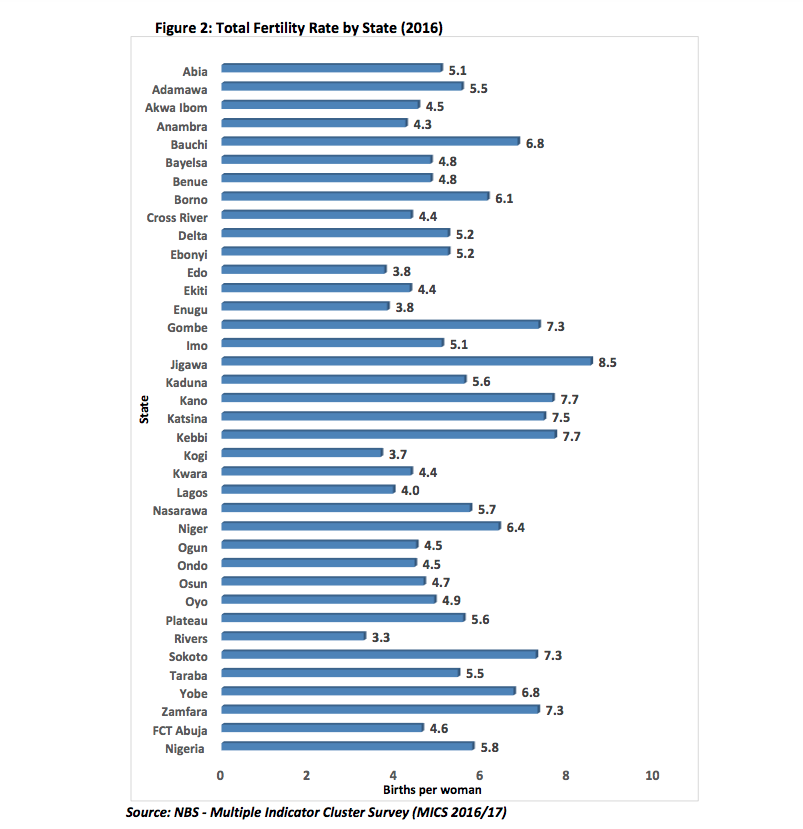
The worst hit in these rural communities are pregnant women and nursing mothers who go through the pains of travelling through rough dusty roads to the next major town where they can get proper medical attention. The journeys may be excruciating sometimes, but they are left with no choice. For those who cannot face the troubles, the available options are to patronise traditional birth attendants, herbalists or nearby healthcare centres where doctors, drugs and basic amenities are non-existent. Even at that, the total fertility rate in the state keeps increasing. From 4.1 in 2013, it jumped to 4.7 in 2016.
45 MINUTES ON A MOTORCYCLE TO DELIVER A CHILD

Thirty-year-old Morufat Ibrahim, a resident of Ponpola village, retorted that life would have been easier for residents of the community if they had a healthcare centre where they can easily seek medical care without travelling through a long distance to treat just malaria.
“Nothing happens here. We are really suffering,” Morufat said. “When I wanted to give birth to my last child eight years ago, I went into labour around 8am. My husband drove me on a motorcycle for 45 minutes to Ede. For most women here, if the baby is coming really fast and they can’t risk the journey to town, they have to deliver at home through midwives. If there’s any complication, they’ll be rushed to Ede or Osogbo.
Advertisement
“We even have to get drugs from the city. When a child is running a temperature and in dire need of treatment, we still have to take him or her to the next major town. The government has not come to our rescue. Anytime we go to another town to access the hospital, you cannot do anything that day again because of the long hours we spend on the road and in that place.”

Meandering on the dust-laden and rough road to Egbedi, a rural community in Egbedore local government area of Osun state, would make your body ache after disembarking from the vehicle that had endured ceaseless screeching and twisting. The only health centre in the town started in a shop in 1994, while the present structure was built in 2001. The woman behind the front desk in the three-room apartment serves as the receptionist, nurse, manager, doctor, technologist and everything else in between. The other two health workers were not usually on the ground but being a resident of the community, she is always on duty — officially and unofficially.
Folasade Lawal, the 48-year-old health technician in charge of Egbedi Health Centre, is called mother by all children in the village as she personally took delivery of most of them. Doctors and nurses don’t work here. With just an obstetrical forceps and scissors, she goes into the small labour room with the expectant mother. She places a touch on her head and holds it firm with a cap. Then, work begins. If the delivery falls at night, relatives of the woman in labour runs to her house to wake her up. Folashade said she is left with no choice than to rise up anytime of the day to attend to them, even when it is not really convenient.

She said, “I started working here since the inception of the health centre. Later, I was transferred to another town. I came back here in June this year. I was the one who took delivery of so many children in this town. We’ve recorded just one birth this month, which was on September 4. It was a boy. Ante-natal is every Monday, although we have just a patient for now.
Advertisement
“We have never had any issue of complication during delivery because we do refer those with special needs to Erin town which has a good hospital. The town is about 40 minutes from here.”
NO DRUGS, DELIVERY KITS, TOILET, WATER OR ELECTRICITY
Advertisement

When asked the number of babies that have been delivered at the centre, she said they do not have the record. Surrounded by bushes, the facility is battling with so many challenges beyond its frail looks. For emergency situations, there is no ambulance. Patients are bundled into a motorcycle and driven to the next town with a hospital.
“Sometimes, we stop a car going to the next town to carry the pregnant woman to the hospital,” Folashade said. “The only drug we have here is an anti-malaria tablet. Those who need drugs get them from the state capital or bigger towns not too far from here. We only have two beds, then a forceps and scissors for delivery. We are in dire need of delivery kits. We enter the bush at the back of the centre to defecate because there’s no functioning toilet. We have to go and fetch water few meters away and there’s no light as well.”
Advertisement

On a visit, Taiwo Akeem, the last patient to give birth at the health centre on September 4, was carrying the little baby named Fawaz. She used to go to Ido-Osun, a neighbouring town for her antenatal with the hope of giving birth to her baby there. But there was a twist in the plan as the baby unexpectedly announced his coming in the middle of the night. She detailed her experience the midnight she delivered.

“It was in the midnight. My husband put me on his motorcycle and we drove to the health centre. My husband was very restless. He was just pacing up and down. I was with the woman alone in the labour room and I delivered in about two hours. She cleaned me up and we went home in the morning.”
Advertisement
‘I GET SCARED THAT I MIGHT DIE ON THE JOURNEY TO THE NEXT TOWN FOR TREATMENT’

Adewunmi Mujidat, who has been living in Egbedi for the past 30 years, said Folashade took delivery of her five children, including Kafayatu who was born in 1996 with speech and hearing impairment. “I gave birth to her in the morning. It wasn’t easy then but I had a safe delivery,” she said.
Often times, Mujidat battles with malaria which renders her bedridden for days. When it becomes severe, she boards the next motorcycle to Ilobu, a nearby town where she’d stay until she’s healthy enough to return to her work. Usually, she wakes up as early as possible to prepare food for her family and by 9am, she sits under a shed in front of her house to fry garri.
“The last time I had malaria, Folashade was taking care of me until it became worse. So, I went to Ilobu where I took about eight drips in the hospital. When I get sick in the night, my head will start aching and I will start getting scared that I might die in the journey before I get to the next town,” she said.

As for Modupe Clement, the only antenatal patient at Egbedi health centre, her husband would take her on a motorcycle to Ilobu anytime the stomach pain she has been struggling with resurfaces.
She said, “I can experience the pain from morning till evening when it comes. I’d cry and writhe in pain. I don’t know the cause of the pain. When I went for scanning in a hospital in Ilobu, they said my child is doing fine. But the doctor said I should go for another scan at Ido-Osun. So, I visit those two towns frequently just to get my body in order.”
HEALTH CENTRE WITHOUT PATIENTS
At Agodo village, residents prefer to travel several kilometers to Osogbo, the state capital, to give birth than to risk their lives at the community’s only health centre where there are no delivery kits and the health officials “rely on God’s help” during deliveries. Founded in 2009 with little equipment, the fortune of the clinic became worse such that it has not recorded any birth since the beginning of the year despite the fact that women in the village get pregnant and deliver.
The only official on duty, Mansur Ibrahim, a 30-year-old health technician, said the centre has only one ante-natal patient presently although she is not always punctual. Since the establishment of the health centre, Ibrahim said they have had 50 births although there was no record to show for it. The centre neither has an electricity connection nor a water system for patients. They fetch water from wells.

“The last time we delivered a baby here was last year. They prefer to travel to the state hospital to give birth because we don’t have enough equipment. Only God is helping us here during deliveries. That’s why we swiftly refer complicated cases to the state hospitals.”
WHY DOCTORS HARDLY WORK IN RURAL AREAS

In a telephone interview with TheCable, Adegboye Isawunmi, a consultant at the department of obstetrics and gynaecology at the Ladoke Akintola University of Technology (LAUTECH) teaching hospital, Osogbo, said doctors and midwives cannot work in rural areas because of poor remuneration. Whereas most of the cases they handle at the teaching hospital are being referred from rural areas, they prefer to work at specialist or teaching hospitals where the pay is higher.
“One of the reasons why the health workers don’t want to go rural areas is the remuneration. If someone is not paid well, he or she will look for a way to work in the tertiary hospitals,” he said.
“There was a time that the minister of health went to one place and found out that there were more doctors in the teaching hospital than the whole doctors employed by that state. There should be a general salary for all doctors, just like we have for judges; so that doctors won’t say I want to work in certain areas. Some of them leave the local communities to get the job of a lower cadre at teaching hospitals because of the remuneration.

“Most of our midwives are working in urban areas. They are not being employed to primary health centres and we know that most of our population is in rural areas. One of the reasons why maternal mortality is still high is because of lack of skilled personnel to attend to our pregnant patients during labour.
“Most of these health centres are manned by unskilled workers. Although most of them attend school of health technology but they are not exposed to practical aspects of attending to patients in labour. They don’t have what they can use to measure blood pressure, because hypertensive disorder is one of the reasons we have increase in maternal death. Most of the skilled workers will not refer the patients on time until it has gone out of hand.”
Isawunmi added that even the state specialist hospitals may not be able to do more than one or two caesarian sections in a day because they lack facilities.
DESPITE HUGE HEALTH BUDGETARY ALLOCATION, MORE WOMEN ARE DYING
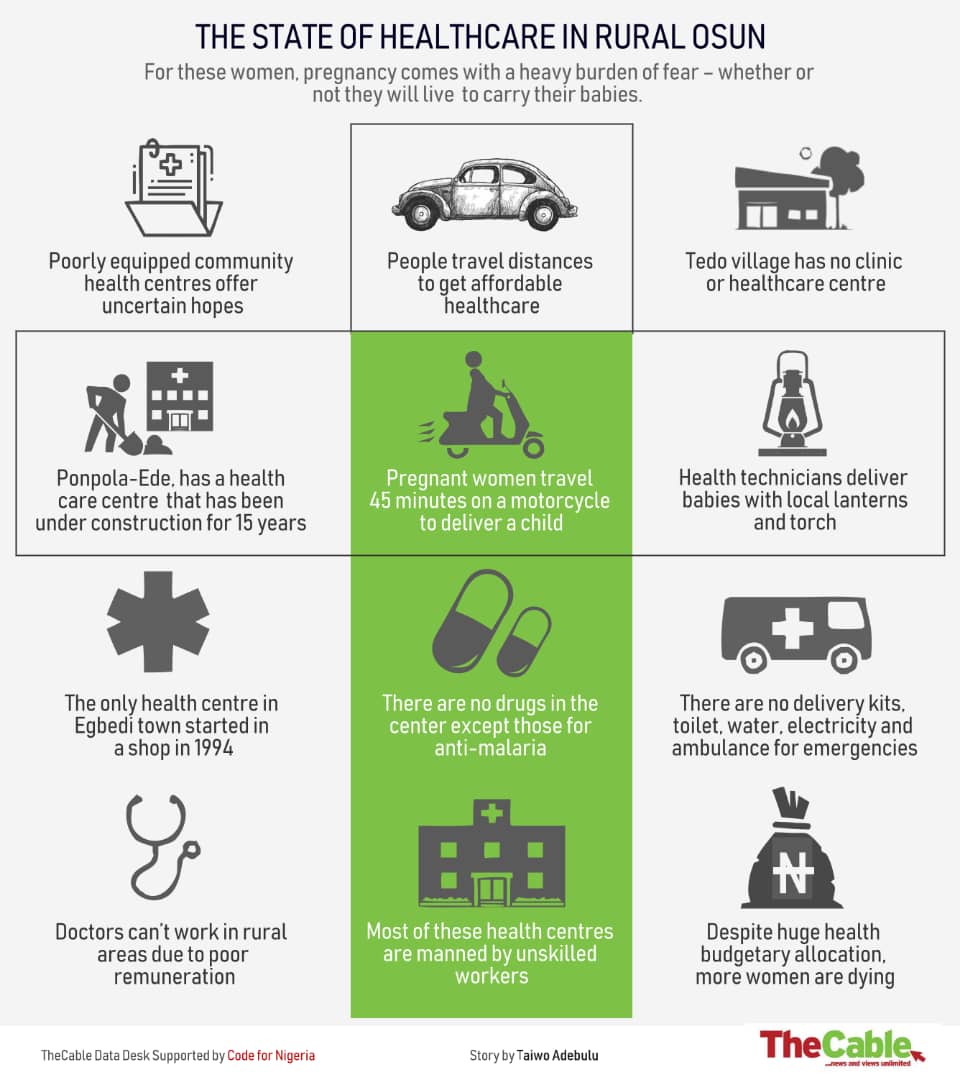
From N257bn in 2016, N304bn in 2017 to N340 in 2018, the allocation for the health sector in Nigeria keeps soaring. Even with the multi-billion naira annual budgets, available data shows that the country is not in any way improving on maternal mortality rate (MMR) as more pregnant women and nursing mothers face huge difficulty with accessing basic healthcare especially in the rural areas.
A joint report by the World Health Organisation (WHO), United Nation Population Fund (UNFPA), United Nations Children Fund (UNICEF) and World Bank showed that Nigeria recorded 58,000 deaths from maternal mortality in 2015.
As things stand presently, Nigeria has the second highest burden of maternal mortality in the world, and contributes about 15 percent of the annual total global deaths which represent two percent of the global population. According to the World Bank, MMR in Nigeria is still as high as 821 per 100,000 live births, while the Nigerian Demographic and Health Survey (NDHS) reports for 2008 and 2013 revealed that Nigeria achieved practically no reduction in MMR.
In March, at the 18th general membership meeting on reproductive health supplies coalition (RHSC) in Brussels, Belgium, experts disclosed that while global maternal mortality dropped by about 43 percent since 1990, Nigeria still ranked highest among sub-Saharan African nations with high maternal deaths.
Bill Gates, co-founder of the Bill and Melinda Gates Foundation, had ranked Nigeria as one of the most dangerous places in the world to give birth and 4th country with the worst maternal mortality rate ahead of Sierra Leone, Central African Republic and Chad.
As of 2015, Folasade Ogunsola, a professor of medicine, said assuming no doctor leaves the country, it will still take the country 100 years to the have the number of doctors it needs.
Ogunsola said this while delivering a lecture at the opening of a capacity development programme for medical staff in Nigerian universities. The lecture was organised by the National Universities Commission (NUC) in Abuja.
“We will need about 237,000 medical doctors and we have about 35,000 working in the country today,” the professor had said.
IS THERE A WAY OUT?

Despite the overwhelming challenges in these rural communities, Rafiu Isamotu, the state commissioner for health, said the current administration in the state has made progress in the health sector. He insisted that all the health centres in the state have doctors, nurses, pharmacists and fully equipped with medical tools.
“Maternal mortality in my state probably mirrors what we have nationally or slightly better. However, this is not desirable, we want to improve and be better than this,” Isamotu said.
“We have done pretty well in this area. 28 existing primary health centres upgraded, 90 new primary healthcare centres were built and fully equipped. 33 solar-powered boreholes and new 90 motorized boreholes constructed for state health centres across the state, state government supplied new medical equipment to 208 primary health centres in the state.
“As far back as 2014, we purchased 100 hand-held scanners which we distributed to our health centres in our rural areas. Basically the ultrasound scanners are user-friendly such that our midwives and community health workers are able to scan our pregnant mothers to be able to determine common complications like breech presentation, low lying placental, little dry amniotic fluid etc and make appropriate referrals to secondary and tertiary facilities. This measure has actually saved many pregnant women from preventable deaths.
“This year, 2018 we procured Kiwi which is a hand-held device that we use to deliver pregnant women. This is done to reduce unnecessary cesarean sections. There are known cases though that have absolute indications for CS.
“We had trained traditional birth attendants in rural areas such that they will know their limits and imbibe modern day basic obstetrics practice.”
When asked why there are no qualified medical personnel in rural health centres, Isamotu reiterated, “There’s none of our health centre that does not have either a doctor, a nurse, community health worker or their equivalent, pharmacist, relevant technicians etc.
“However, this does not mean that we have satisfied WHO recommendation as regards staffing of our facilities. Our government will still engage staff before we exit.”
Isaac Adewole, minister of health, stated that it is possible for the country to achieve below 100 maternal mortality rate by 2030 if the government can strengthen its social intervention programmes. He said this last year in Abuja while inaugurating the task force on accelerated reduction of maternal mortality in Nigeria.
The minister maintained that there is a strong correlation between maternal mortality and level of social and economic development of any country. With the declaration that Nigeria has taken over as the country with the highest number of extremely poor people, that makes the future bleaker.
For Isawunmi, the government needs to train more midwives to go to rural communities where women are battling with poor access to health services.
“The Society of Gynaecology and Obstetrics of Nigeria (SOGON) is coming up with voluntary obstetrics services such that some of the obstetricians around that are in the urban areas would go occasionally to some of these primary health centres in rural areas.”
However, in the face of dire economic development and failing healthcare system, the road to achieving the sustainable development goal of ensuring universal health coverage is still a long way to go as more women in rural settlements battle to survive with childbirth.
Photos by Ibrahim Mansur
Add a comment







