BY NKEIRUKA OBI
Allow me to start with a story. In one of the largest pediatric hospitals in Zambia, I saw theatre nurses warmed up cotton wool on a child undergoing surgery to prevent hypothermia. I have seen a midwife deliver a baby with the flashlight of a phone tied to the forehead to illuminate the delivery room. These experiences are common, but are they the most appropriate methods?
Surgical care saves lives, prevents disabilities and is the bedrock of functional health systems, addressing the full extent of human disease. When properly resourced, it plays a fundamental role in every hospital and health facility – resulting in stronger health systems overall – providing a clear pathway towards Universal Health Coverage (UHC). Yet, optimally functioning surgical systems have failed to materialise in many under-resourced countries.
I recently attended the International Symposium on Strengthening Surgical, Obstetric and Anaesthetic Care Systems in Africa which was hosted in Senegal, led by Mercy Ships. It gathered ministers of health from across the continent for authentic and thought-provoking reflection of how important strengthening surgical and anaesthesia care in Africa is.
Advertisement
First and foremost, healthcare alone cannot change health. There’s a saying that goes, “a single finger is not enough to clean the face”. We have seen that it is no longer an option, partnerships that foster accessibility, accountability, and transparency in providing safe and quality surgical and anaesthesia care in LMICs are paramount. It is crucial to synchronise efforts for multi-stakeholder engagement. Private and public stakeholders must recognise the enormous health toll and financial burden of surgical disease and avoid working in silos.
Secondly, the time has come for streamlining processes at policy level. Policy implementation and regulatory frameworks must be designed to attract the use of finance and new technologies in ways which generates sustainability. It is only through a cross-sectoral approach that we can achieve the primary goal of strengthening surgical systems in Africa.
We can’t afford to let landmark global commitments to universal health coverage fall by the wayside. We must hold ourselves as expert-leaders responsible for building and safeguarding systems that leave no one behind, starting with health, and unlock dividends for wellbeing and progress everywhere. Let’s balance the scale of equity in meeting everyone’s needs, no matter who or where they are.
Advertisement
The neglect of surgical care has devastating social and economic consequences especially for Africa with rapidly growing population of 50% children and adolescents. The data is well established (Lancet Commission on Global Surgery). The political mandate has been established with WHA Resolution 68.15.
National Surgical Obstetrics and Anaesthesia Plan (NSOAP) is identified as an entry point. The global surgery community and its partners are waiting to support its implementation in strengthening the capacity of the local SOA workforce with scalable and sustainable resources to enable them offer culturally appropriate care for our patients and to extend their care even beyond without the risk of brain drain.
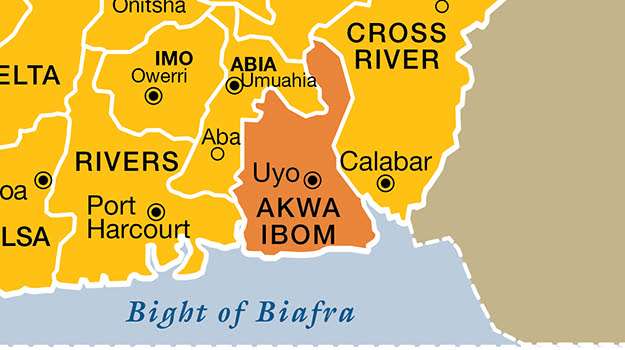
Nigeria NSOANP implementation, an example with Smile Train support, indicates that surgical services can be scaled to community level, with the right investment in leadership and governance, resource mobilisation and planning (funding, workforce and infrastructure, research prioritisation for evidence-based solution towards patient preparation and treatment accessibility to these essential services). There is also a need to prioritise pediatric surgical care.
Smile Train is a global cleft-focused non-profit, centred on improving health equity around the world by offering those born with cleft lip and palate access to safer surgeries and comprehensive cleft care in LMICs. In Africa, over 160,000 patients have benefited from our programmes across 41 countries…nutrition, psychosocial support, anaesthesia, surgical and nursing care, speech therapy, orthodontics, biomed SIRT, research funding, ENT, oral health.
Advertisement
We have made significant investment in surgical and anaesthesia training by collaborating with accreditation bodies such as the West African College of Surgeons (WACS) and the College of Surgeons of East, Central and Southern Africa (COSECSA) and building Africa’s first Cleft Centre of Leadership and Excellence in Ghana.
The task is enormous. As we climb this mountain, we acknowledge its fair share of obstacles. From limited funding (national budgets), roadblocks in trade (importation of surgical equipment), education (huge deficit SOA workforce density), lack of infrastructure, lack of transparency, we remain positive and resolute that the deliberations today will open more in-roads to ensuring equitable access to care and better health outcomes for those at greatest need in all Africa countries.
As we urge governments to take appropriate actions to prioritise health care, to strengthen local health systems through investment, resources and local capacity building and to use data to inspire research, innovate, improve systems and maximise impact, let us continue to work together and ensure that local surgical teams are equipped to deliver safe, quality, people-centred care in their own communities. Smile Train is here to collaborate and partner.
Obi is the vice-president and regional director for Africa at Smile Train
Advertisement
Views expressed by contributors are strictly personal and not of TheCable.
Add a comment